
Europeans have a hard time holding their drink, this continent is topping the drinking charts globally. Is it nature, culture, or a policy issue? We discuss alcoholism on today’s Standard Time.
The rush to find a COVID-19 vaccine has resulted in myriad products rather than medical strategies. In the West, mostly private labs are behind what has become a precious commodity. How did public health and money become contractually tied to privately owned medicine?
In 1955 a journalist asked US doctor Jonas Salk who owned the patent to the polio vaccine he had just developed. He replied, somewhat provocatively, ‘The people, I would say. There is no patent. Could you patent the sun?’ Polio was then one of the most terrifyingly lethal diseases and Salk’s rhetorical question was related to an idea of public health that unfortunately no longer exists.

Photo by pedro1997alves via Pixabay
Today, we are facing a health crisis linked to the SARS-CoV-2 virus, which in one year has claimed more than two million lives worldwide. From the very beginning of the pandemic, hopes of embracing our loved ones again were placed in the development of a safe and effective vaccine: a kind of Holy Grail of public health. Although vaccines are second only to clean drinking water in reducing mortality from infectious diseases, today they are linked more to market logic, ideologies and geopolitical interests than to health system needs.
The neoliberal narrative has taken for granted that the private sector offers the best guarantee of continuous innovation. However, during the pandemic, the shady side of this system has become visible.

This article was originally published in Eurozine’s Italian partner journal il Mulino.
Due to the high cost of developing vaccines and the rapid actions of rich countries placing advance orders, more than 85 developing countries may not have access to the vaccine before 2023. Indian economist Jayati Gosh speaks of ‘vaccine apartheid’.
Even the EU, rich as it is, has been left without pre-ordered doses, because it negotiated lower prices than some countries. If vaccines are such fundamental tools for collective health, how and why have western countries completely delegated their production to the private sector?

Photo by Daniel Schludi on Unsplash
Following successes within bacteriological science in developing serums against rabies and then diphtheria at the beginning of the twentieth century, new research institutes were needed to provide sera and vaccines. Some countries looked to private laboratories: the Sclavo Institute, Italy, is one example. Others, such as Denmark and Sweden, established public institutions linked to health ministries or municipal public health laboratories.
A common effort to protect public health connected European producers of public and private vaccines in the 1960s and ’70s, who exchanged their knowledge and expertise. However, in the ’80s, economic, political and technological pressures began to slowly erode the public sector.
The last few public institutions that remained afterwards were dismantled in the 1990s and 2000s. In 1993 a Dutch biotechnology company acquired Sweden’s production department once it had been separated from the national lab’s other functions. The pharmaceutical giant Johnson & Johnson then bought out the facility.
In 2009 the Dutch government decided to stop its direct production of vaccines, divided up institutional departments and, a few years later, an Indian company bought the production facilities. The sale of its research department – the last to remain – is still a matter of debate.
Today, western Europe has no public vaccine producers unlike certain post-socialist central and eastern European countries such as Serbia and Romania. The most common explanation is deemed financial. For example, the former Dutch Health Minister Ab Klink highlighted that the cost of producing vaccines for the small Dutch population (around 180,000 births per year) was excessive.
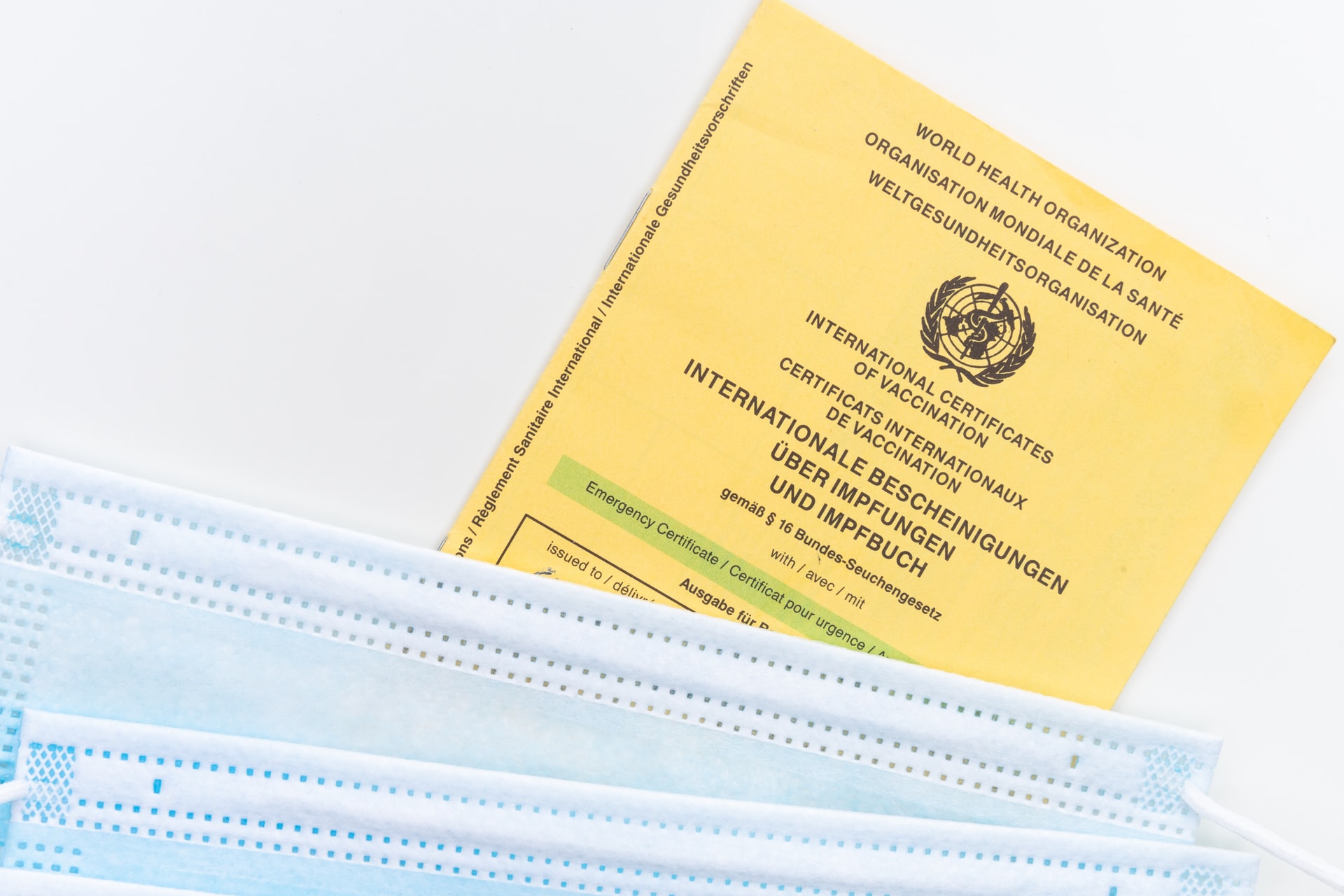
Photo by Markus Winkler on Unsplash
In reality, economic reasons are only part of a more complex story. If we follow the developments of science and technology on the one hand and ideological changes on the other, a scenario emerges in which multiple dynamics intertwine. In the 1960s and ’70s, vaccine technologies, using methods of attenuation and inactivation,1 had to safely preserve and manage cultures of dangerous pathogens, making large and complex laboratories indispensable. By the 1980s, new techniques of genetic manipulation, along with a series of US-implemented public policies, encouraged many scientists to move from university laboratories to small biotechnology companies.
Company knowledge became embedded in increasingly dense networks of patents. As noted by Berkeley economists Mowery and Mitchell, while two patents sufficed to develop 27 new vaccines in 1983, a decade later, Smithkline Beecham (now GlaxoSmithKline) had to collect 14 patents to produce and market a single recombinant DNA vaccine against hepatitis B. ‘Knowledge’ and the inevitable cooperative relationships in research had become ‘intellectual property’. Limiting public interest in favour of individual rights halted the free exchange, development and adaptation of scientific knowledge.
As private and public producers of traditional vaccines had no experience of biotechnology techniques, big pharmaceutical companies began to acquire new companies with the skills and patents they needed. More and more companies merged during this period of acquisition, transforming much of the pharmaceutical market into a transnational, oligopolistic field.
Simultaneously, public institutions were hollowed out. Since they were excluded from the new patent market, unable to play by the new rules, the view spread that public sector producers no longer had the resources, autonomy from political interference and skills to produce good quality vaccines.
A young Indian girl receiving a dose of oral polio vaccine by a trained healthcare worker. Original image sourced from US Government department: Public Health Image Library, Centers for Disease Control and Prevention. Public Domain CC0 Image Photo via rawpixel
Though still interwoven with public research networks, neoliberalism has redesigned the pharmaceutical-health sector. Barriers and fences limit the circulation of knowledge and reduce the public health system’s capacity to react to real emergencies. The western state and its political class no longer see the provision of essential tools for public health such as vaccines as their direct responsibility.
If this pandemic is a wake-up call, and other zoonotic diseases emerge, as they surely will, the renegotiation of public institution participation in vaccine production becomes all the more urgent. Governments can no longer be left unprepared or held hostage to the market logic of the private sector, where inequalities in access to life-saving technologies are considered acceptable.
While inactivated vaccines are produced by growing the bacterium or virus in culture media, which is then inactivated with heat and/ or chemicals, attenuated vaccines use a weakened (or attenuated) live form of the germ that causes a disease.
Subscribe to know what’s worth thinking about.

Europeans have a hard time holding their drink, this continent is topping the drinking charts globally. Is it nature, culture, or a policy issue? We discuss alcoholism on today’s Standard Time.

There are times when reacting on instinct surpasses consciously weighing up decisions. But what lies behind precognition? Tracing gut feelings back along their evolutionary path leads to C. elegans. What might the inconspicuous worm, with its belly full of serotonin, help illuminate about scientific scepticism, ‘happy pills’ and experienced intuition?